30 Mar 2015
Some notes from SGM 2015:
Microbiome session
Diabetes, obesity and gut microbiota
Patrice Cani
1. Microbiota-host interactions play a major role in obesity
2. Intestinal MyD88 is a sensor switching host metabolism during fat feeding
3. Endocannabinoids are key players involved in the microbiota-host interaction
Intestinal epithelial MyD88 is a sensor switching host metabolism towards obesity according to nutritional status
http://www.nature.com/ncomms/2014/141205/ncomms6648/full/ncomms6648.html
The endocannaboid system links gut microbiota to adipogenesis.
http://www.ncbi.nlm.nih.gov/pubmed/20664638
Adipose tissue NAPE-PLD controls fat mass development by altering the browning process and gut microbiota
http://www.nature.com/ncomms/2015/150311/ncomms7495/full/ncomms7495.html
Test from Torsten, not at SGM. Looked like an interesting talk!
Bacterial persisters
Sophie Helaine
Many species form persisters - highly tolerant to Abx. Persister cels represent a small sub-population caused b phenotypic switch. E. coli in vitro persisters are non-replicating bacterial cels.
Background:
http://www.nature.com/nrmicro/journal/v9/n7/full/nrmicro2601.html
Bacterial persisters: formation, eradication, and experimental systems
http://dx.doi.org/10.1016/j.tim.2014.03.008
Internalization of Salmonella by Macrophages Induces Formation of Nonreplicating Persisters
http://www.sciencemag.org/content/343/6167/204
5-10% of the non-replicating bacteria resume growth.
Toxin-antitoxin systems related to persistence of E. coli in vitro.
http://www.pnas.org/content/108/32/13206.abstract
Thoughts: how to link dead/alive/persistence state to metagenomics data (single cell RNA-Seq?)
http://www.ncbi.nlm.nih.gov/pubmed/20890840
http://www.ncbi.nlm.nih.gov/pubmed/16085863
Stephen Bentley
Pneumococcus human host-restricted, usually lives in nasopharynx.
No overall change in species prevalence post-CV7. Subtle effects on resistance- generally remain stable.
Population genomics of post-vaccine changes in pneumococcal epidemiology
http://www.nature.com/ng/journal/v45/n6/full/ng.2625.html
MDR not secret of success for antimicrobial resistance.
Association between high admixture and AMR previously shown
http://www.ncbi.nlm.nih.gov/pubmed/19520963
Consistency in recombination hotspots between lineages
http://www.nature.com/ng/journal/v46/n3/abs/ng.2895.html
Non-typeable clone most efficient recipient of DNA by recombination
http://www.ncbi.nlm.nih.gov/pubmed/25480686
MGEs in pneumococcal AMR
http://www.nature.com/ncomms/2014/141119/ncomms6471/abs/ncomms6471.html
Prophage insertion in comYC genes blocks recombination in IC1 - !
Variable recombination dynamics during the emergence, transmission and ‘disarming’ of a multidrug-resistant pneumococcal clone
http://www.biomedcentral.com/1741-7007/12/49
Fleming Prize Lecture
Michael Brockhurst
Sex, Death and the Red Queen
http://www.sciencemag.org/content/333/6039/166.figures-only
Running with the Red Queen: the role of biotic conflicts in evolution
http://rspb.royalsocietypublishing.org/content/281/1797/20141382
Antagonistic coevolution accelerates molecular evolution.
http://www.ncbi.nlm.nih.gov/pubmed/20182425
Coevolution accelerates molecular evolution
Coevolution drives greater between-population divergence
In clinical samples:
Divergent, Coexisting, Pseudomonas aeruginosa Lineages in Chronic Cystic Fibrosis Lung Infections.
http://www.ncbi.nlm.nih.gov/pubmed/25590983
Highly parallel evolution of LES lineages: mexAB-oprM, creBCD, ampC, lasR, oprD, pmaA, etc. etc.
Rapid turnover of diversity within patients
http://www.ncbi.nlm.nih.gov/pubmed/21297072
Evidence for changes in diversity during exacerbations, and evidence for lineage ‘switching’ over time.
Single strain bacterial populations high diverse
Most diversity is present in individual sputum samples
Diversity in clinically important traits like AbR and secreted molecules
Genetic data shows parallel evolution and patient-patient transmission.
What’s driving diversification in CF lungs? (Immune system Abx, species interactions, etc.)
Phage?
http://www.nature.com/ismej/journal/vaop/ncurrent/full/ismej2014223a.html
Evolutionary adaptation to ASM environment by:
- loss of motility structures esp flagellum
- mtabolic and biofilm changes
Adding temperate phages to artifiicial sputum medium selects for a different set of mutations than seen in CF in-host evolution, e.g. pili, Type 6 secretion, flagellum, quorum sensing, etc.
Phage insertions cause several parallel mutations.
AMR in South Asia
Stephen Baker
Return to pre-AMR era
http://www.sciencemag.org/content/347/6226/1064.full
S. Typhi: monomorphic
Emergence of fluoroquinolone resistance, independent hyrA mutations.
Fitness benefits in fluoroquinolone-resistantSalmonella Typhi in the absence of antimicrobial pressure.
http://elifesciences.org/content/2/e01229
A high‐resolution genomic analysis of multidrug‐resistant hospital outbreaks of Klebsiella pneumoniae
http://embomolmed.embopress.org/content/early/2015/02/17/emmm.201404767.abstract
K. pneumoniae is exceptional coloniser of surfaces, tubes, etc.
K. pneumoniae outbreak - two distinct lineages, acquired blaNDM-1.
Longitude Prize
The test must: identify when antibiotics are needed and if they are which ones to use.
Test must be: needed, accurate, affordable, rapid (<30 min), easy-to-use, scalable, safe, a prototype must be available.
Easy-to-use: minimally invasive, easy to dispose, long expiration, heat stable, withstand transportation, minimum maintenance etc.
Modelling Clostridium difficile infection
Caroline Chilton
In vitro human gut model: tripe chemostat system arranged in weir cascade, primerd with faecal slurry, validated against the caecal content of sudden death victims.
Antibiotics knock down Bifidobacterial populations. Bacteroides not affected by clindamycin but effected by vancomycin.
16S profiling matches colony counts well.
Observed diversity highest pre-antibiotic, lowest with recurrence. Fidaxomicin less effect on diversity than others.
http://link.springer.com/article/10.1007%2Fs002489900072
Biofilm human gut model using rods
http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0088396
Ebola
Mutation rate and genotype variation of Ebola virus from Mali case sequences
http://www.sciencemag.org/content/early/2015/03/25/science.aaa5646
Epidemiological and viral genomic sequence analysis of the 2014 Ebola outbreak reveals clustered transmission
http://cid.oxfordjournals.org/content/early/2014/12/12/cid.ciu1131.short?rss=1
Michael Tunney, QUB
CF microbiome: culture studies shows significant numbers of anaerobes (similar to P. aeruginosa).
Healthy airway microbiome quite similar to CF microbiome — Streptococcus, haemophilus, Rothia etc. but don’t see Pseudomonas, Burkholderia etc.
Diversity decreased in CF
Diversity positively correlated with lung function
http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0045001
Decade-long bacterial community dynamics in cystic fibrosis airways
http://www.pnas.org/content/109/15/5809.short
Lung explant microbiome study
http://www.pnas.org/content/109/34/13769/F4.expansion.html
Healthy microbiome cannot be cultured in late-stage CF infection.
William Wade, Oral Microbiome
50% of oral bacteria are uncultivable
Human Oral Microbiome
http://jb.asm.org/content/192/19/5002.full
Most human oral bacteria are found only in the mouth, notable exception Fusobacterium nucleatum.
Intra-oral habitats have characteristic microbiota.
Diet has relatively little effect on oral microbiome.
Why do historical dental samples correlate diet with microbiome? A: Effect of dental hygeiene.
Willlem van Schaik
E. faecium and E. faecalis genetically distinct - penicillin resistant.
E. faecium clade A1 “clinical isolates” - highest mutation rate
E. faecium clade A2 “animal isolates” - medium mutation rate
E. faecium clade B “human commensal” - lowest mutation rate
Phylogeny of closely related strains: gene content mirrors phylogeny. Differences caused by gain/loss of plasmids and phage-like elenents.
Hospital ICU microbiota: characterised by outgrowth of Enterococcus on long stays
Sewage resistome
Zamin Iqbal
75 out of 1607 samples have minor resistance calls
100% resistance correection on MDR S. aureus
Ebola virus
Prior to 2013: ~20 outbreaks, ~1,600 deaths, 25-90% mortality rate, 5 Ebolavirus species
Filovirus epidemic in 1956 in Bili, DRC - first Ebola outbreak?
http://www.thelancet.com/journals/laninf/article/PIIS1473-3099%2815%2970092-7/abstract
Emergence of Ebola
http://www.nejm.org/doi/full/10.1056/NEJMoa1404505
25000 cases, 10000 deaths
Burial rites: involve touching the bodies, washing them. Mobile phone connectivity make it easier to gather more relatives for funerals.
29 Mar 2015
If you are coming to Birmingham for this year’s Society for General Microbiology Annual Conference, welcome! This meeting is pretty big, and the website is curiously unnavigable, so I have put my own personal schedule up here.
A few notables! On Tuesday night there is the announcement of the new SGM journal Microbial Genomics in Hall 3 which I am pleased to be serving on the editorial board. Lots of tweeps are likely to be there. Straight afterwards we will head to a local pub for a “tweet-up”.
On Wednesday morning we will be launching our new BBSRC-funded grant MicrobesNG over at the stunning new Library of Birmingham which is well worth a visit if you haven’t been in. MicrobesNG aims to provide a very different type of sequencing service, specifically tailored to the needs of microbiologists. We will be running two sessions explaining exactly what we are doing, with refreshments provided. Please sign-up over at the website if you would like to come along!
In terms of scientific sessions I will be mainly hopping between the antibiotic resistance session and the microbiome session, with a few detours for prize lectures and hot genomics lectures. During the breaks I will be over on the MicrobesNG trade-stand. Look forward to saying hello!
And if you are interested in nice places to eat in Birmingham, the Guardian just did a nice piece on cheap eats and we also keep a map of places we like over on my food blog.
Monday 30th
BI05 Microbiome in Health and Disease
09:00 The human microbiome in health and disease Julian R. Marchesi (Cardiff University, UK)
09:30 Diabetes, obesity and gut microbiota Patrice Cani (University of Louvain, Belgium)
BI21 Antimicrobial resistance
11:00 Salmonella persisters in the host Sophie Helaine (Imperial College London, UK)
11:30 A population genomics view of pneumococcal antimicrobial resistance Stephen Bentley (Wellcome Trust Sanger Institute, UK)
12.10 Fleming Prize Lecture – Rapid microbial evolution: From the lab to the clinic and back again Michael Brockhurst (University of York, UK)
14:00 Antimicrobial resistance issues and selective pressures in South East Asia Stephen Baker (Oxford University, UK)
14:30 Offered paper - Detection of NDM-1 positive pathogens and genes in the Ganges River associated with seasonal human migration to pristine areas David Graham (Newcastle University, UK)
14:45 Offered paper - Broad spectrum antimicrobial peptides derived from a bovine rumen Linda Oyama (Aberystwyth University, UK)
15:00 Small World Initiative Paul Hoskisson (University of Strathclyde, UK)
15:15 Longitude Prize Tamar Gosh (NESTA, UK) and Laura Piddock (University of Birmingham, UK)
BI05 Microbiome in Health and Disease
16:00 Metabolomic characterisation of the gut microbiome and disease Elaine Holmes (Imperial College, London)
16:30 Diet and the gut microbiome Yolanda Sanz (National Research Council, Spain)
17:00 Modelling Clostridium difficile Infection Caroline Chilton (University of Leeds, UK)
Tuesday 31st
BI01 Natural and Unnatural Virus Evolution
09:15 Offered paper - Elucidating variations in the nucleotide sequence of Ebola virus associated with increasing pathogenicity Isabel García-Dorival (University of Liverpool, UK)
BI05 Microbiome in Health and Disease
09:30 Lung and normal airway microbiota and implications for cystic fibrosis Michael Tunney (Queen’s University Belfast, UK)
10:00 The oral microbiome in health and disease Wiliam Wade (Barts and the London School of Medicine and Dentistry, UK)
11:00 Klebsiella pneumoniae population genomics and antimicrobial resistance Kathryn Holt (University of Melbourne, Australia)
11:30 Emergence of resistance in tuberculosis: Clinical and in vitro studies Stephen Gillespie (University of St Andrews)
BI21 Antimicrobial resistance
14:00 The human gut as reservoir for antibiotic resistance genes and opportunistic pathogens Willem van Schaik (University Medical Center Utrecht, Netherlands)
14:30 Mathematical modelling as a tool to explore unexpected aspects of antimicrobial resistance Robert Beardmore (University of Exeter, UK)
15:00 Offered paper - Displacement of stable bacterial plasmids by a self-transmissable pCURE plasmid as a means of reducing antibiotic resistance gene load
Alessandro Lazdins (University of Birmingham, UK)
15:15 Offered paper - Enabling genomic-based antimicrobial susceptibility predictions in the clinic: case studies for S. aureus and M. tuberculosis
Zamin Iqbal (University of Oxford, UK)
16:00 Offered paper - The infant airway microbiome in health and disease impacts later asthma development Kathryn Holt (University of Melbourne, Australia)
16:15 Offered paper - The Effects of Novel Dietary Interventions on Campylobacter and the Caecal Microbiome of Broiler Chickens Adrian Horton (Aberystwyth University, UK)
16:30 Phylogenetic assessment of microbiomes – how do we make it more democratic? Jeron Raes (Vrije University, Belgium)
17:00 Microbe-host interactions in chronic intestinal inflammation - microbial dysbiosis versus pathobiont selection Dirk Haller (Tu Munich, Germany)
17:35 Hot Topic Lecture: Ebola virus Hall 1
18:30 New Journal Announcement: Microbial Genomics Hall 3, ICC Birmingham
18:45 Straight after announcement: Tweet-up!
Wednesday 1st April
Over at the Library of Birmingham we will be hosting two workshops in the morning (09:00 - 10:15 and 10:30 - 10:45) to launch our new microbial genome sequencing and strain archiving service, MicrobesNG. Head over to the website to sign-up if you want to find out more!
12:10 Marjory Stephenson Prize Lecture – What’s the host and what’s the microbe? ICC Birmingham Robin Weiss (University College London, UK)
BI21 Prokaryotic Genetics Forum
14:00 Bacterial protein glycosylation - never say never with bacteria Hall 11a Brendan Wren (London School of Hygiene and Tropical Medicine, UK)
14:30 Offered paper - Identification of DNA uptake sequences in Neisseria gonorrhoeae that are intrinsic transcriptional terminators using bioinformatics supported by RNA-seq Sabrina Roberts (Kingston University, UK)
14:45 Offered paper - Regulation of fimbrial genes in Enteroaggregative Escherichia coli Muhammad Yasir (University of Birmingham, UK)
15:00 Offered paper - Investigating the fitness implications of phase variation rate in Campylobacter jejuni using a cyclical selection assay based on phage and human sera Jack Aidley (University of Leicester, UK)
15:15 Offered paper - Expanding your horizons: phenotypic and genomic insights into very broad-host range phages isolated from Lake Michigan Siobhan Watkins (Loyola University Chicago, USA)
16:00 Offered paper - Evolution of Staphylococcus aureus after a human to livestock host-jump event Rodrigo Bacigalupe (The Roslin Institute, UK)
12 Mar 2015
Tuesday, 5th May 2015
WG04, Biosciences
University of Birmingham
B15 2TT
Building R27 on Campus Map: http://www.birmingham.ac.uk/Documents/university/edgbaston-campus-map.pdf
http://www.birmingham.ac.uk/contact/directions/getting-here-edgbaston.aspx
Suggest parking in North East car park (B15 2SA), 10 minutes walk from Biosciences.
For those arriving by train, the venue is a few minutes walk from University (Birmingham) train station which is 10 minutes from Birmingham New St. When buying your ticket, ensure that the destination is University (Birmingham).
13:00 - 16:30, then straight off for a curry.
“Revenge of the Commonwealth”
I’d quite like to bring this balti and bioinformatics meeting
“back to basics”. The last few have got quite large, and talk-
heavy, whereas I originally envisaged these meetings as a community
forum for bioinformaticians to talk openly about problems they were
encountering, and get the benefit of a diverse group of people
struggling with their own problems. And hopefully to make strong connections
that would outlast the meeting and lead to collaborations or
self-help groups etc.
But we will have great talks too, and this is your opportunity to answer
the question which is very much to the front of any British person’s
mind, namely: which of the ex-colonies are managing better without
us, Australia or Canada?
So I am going to limit the number and length of talks down a bit,
and try and carve out some more structured and unstructured discussion
time which would include “solve my problem” sessions and also just more
discussion generally, and perhaps cap the numbers to something
like 50.
Email me suggested topics.
The sign-up form is over heeeeeeeeeere.
Talks:
Jennifer Gardy, British Columbia Center for Disease Control (BC CDC)
Using sequencing to determine if an outbreak is over.
Ana Crisan, BC CDC
Visualizing heterogenous clinical and genomic data to support TB clinical teams
Jen Guthrie, BC CDC
tbc
Torsten Seemann, University of Melbourne
Snippy - rapid variant and core genome construction
Simon Gladman, University of Melbourne
Microbial Genomics Virtual Laboratory
Nick Loman, Univeristy of Birmingham
Update on CLIMB service
02 Feb 2015
The E. coli outbreak metagenomics paper is here:
http://jama.jamanetwork.com/article.aspx?articleid=1677374
MEGAN
MEGAN is both a taxonomic analysis software, and a visualization tool. It is very helpful when ‘mining’ your dataset.
MEGAN takes the results of alignments as input. This alignment information typically comes from BLAST.
Because generating the BLAST format files takes so long, we have precomputed them for you and generated MEGAN5-compatible files.
Load MEGAN (double click MEGAN in its folder).
Start by loading the MEGAN file for sample 2638-H.
For more information on using the various functionality in MEGAN, see the user manual: http://ab.inf.uni-tuebingen.de/data/software/megan5/download/manual.pdf
Please see this videocast for a recap of the MEGAN functionality:
http://www.youtube.com/watch?v=R8dpD_lj6Ts&feature=em-upload_owner
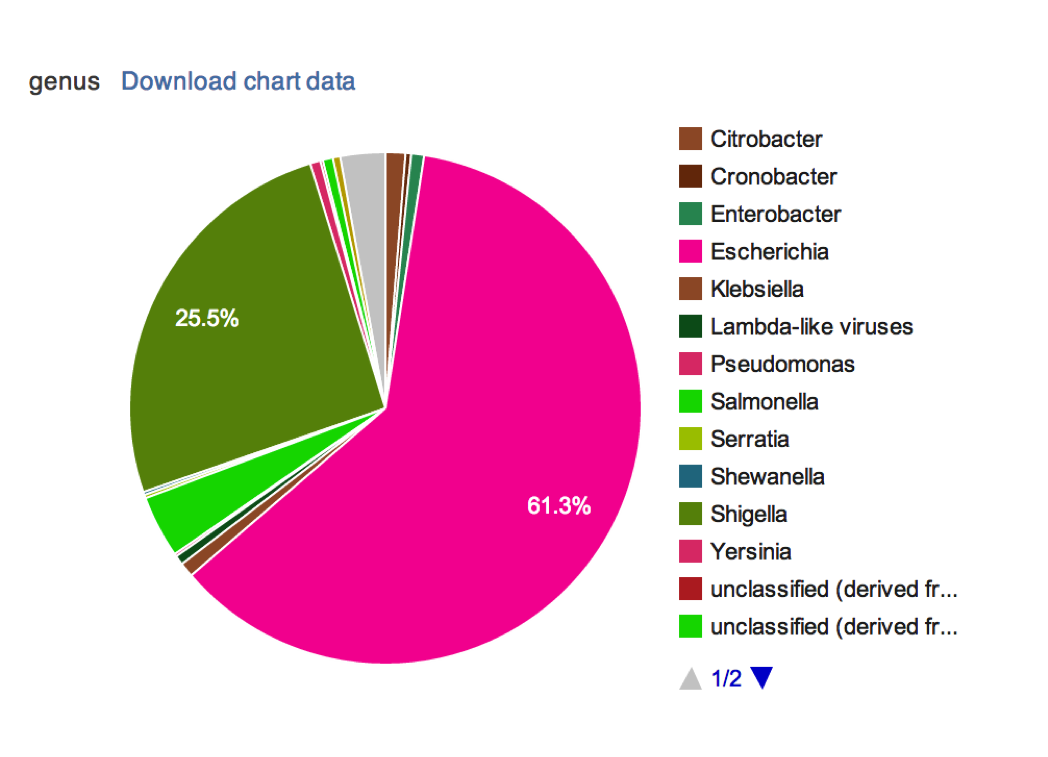
Have a look at the taxonomic assignments:
Which taxon has the most assignments made to it?
What taxonomic level does this taxon belong to?
I have assigned each team four samples to compare:
Find the taxonomic assignments for these samples:
Team 1. Samples 2638, 2741, 1122, 1196
Team 2. Samples 2638, 2535, 1122, 1196
Team 3. Samples 2638, 3014, 1122, 1196
Team 4. Samples 2638, 2741, 1122, 1196
Team 5. Samples 2638, 2896, 1122, 1196
Team 6. Samples 2638, 2840, 1122, 1196
Use the MEGAN inspection mode to compare the samples. Compare at phylum and species order. How do the samples compare? Which samples look abnormal?
Put your results in the Google Docs file:
http://tinyurl.com/webvalley
Inspect the KEGG functional assignments.
Which pathways are conserved across all 4 samples and are complete?
Are there incomplete pathways present, are these surprising? How can they be explained?
Is there evidence of virulence genes being present? Pay particular attention to the categories under “Human Diseases” e.g. “Pathogenic E. coli infection”
Which samples have virulence genes you are worried about? Which patients are affected by the outbreak strain? Are toxins present, which types are they?